The protective effect of perceived social support on psychological health during the COVID-19 pandemic: The case of Gyeonggi province in South Korea
 ; Kunhee Park**
; Kunhee Park** ; Yubin Lee***
; Yubin Lee*** ; Sojin Choi****
; Sojin Choi**** ; Yeongeun Jang*****
; Yeongeun Jang***** ; Myoungsoon You******, †
; Myoungsoon You******, †
Abstract
This study aims to not only examine the protective role of perceived social support (PSS) but also derive practical implications focusing on its effects on depression and embitterment, while considering negative life events (NLEs) during the COVID-19 pandemic.
An online-based, self-reporting survey was administered in January 2022 to 1,000 community residents that were 18 years of age or older in Gyeonggi province, South Korea. The question items included depression, embitterment, PSS, and NLEs. Some covariates, such as sociodemographic characteristics, justice belief, general and governmental trust, and experience of COVID-19 confirmation and self-isolation, were also included. The hypotheses were examined via a hierarchical regression utilizing bootstrap methods.
Higher levels of NLEs during the COVID-19 pandemic are associated with deteriorated levels of depression and embitterment, respectively. The PSS showed significant protective effects on depression and embitterment, respectively, particularly in the consideration of NLEs during the pandemic. The effect of PSS on depression was greater than in that the case of embitterment.
From the analysis of Korea, which applies a range of long-term containment strategies, this study highlights the necessity for the government and communities to develop strategies that can reduce the detrimental impact on psychological health vis-à-vis the significant effects of PSS.
Keywords:
perceived social support, depression, embitterment, mental healthⅠ. Introduction
WHO (2022) described that “the COVID-19 pandemic has had a severe impact on the psychological health and well-being of people throughout the world.” Literature on the coronavirus pandemic reported general population’s increased stress, anxiety, depression, and insomnia (WHO, 2022). The global burden of disease worldwide has elevated by the COVID-19 pandemic to have raised estimation such as major depressive disorder (27.6%) and anxiety disorders (25.6%) during the first year of the pandemic (Santomauro et al., 2021). Nevertheless, studies assessing prolonged psychological effects of coronavirus and its risk factors are still in their infancy.
Previous studies have provided insight that related mental disorders are seeming multifactorial by cause of an aggregation of psychosocial, environmental, and biological factors related to the pandemic (WHO, 2022). Studies have demonstrated that experiencing a stressful life event is a crucial psychosocial factor on one’s deteriorated psychological health both before and after the coronavirus pandemic (Rossi, Jannini, Socci, Pacitti, & Lorenzo, 2021). The described role of negative life events (NLEs) is enlarging individuals’ mental health vulnerability through giving more distress from experiences such as unemployment, workplace conflicts, divorce, personal illness, and the loss or separation experience (Linden, Baumann, Rotter, & Schippan, 2008). The impact of these factors on psychological health and one’s wellbeing could be more severe in the coronavirus pandemic context.
Among the findings about factors associated with levels of psychological health in the prolonged coronavirus pandemic, social support has earned consistent interest as a protective factor (Scheid & Wright, 2017; Szkody, Stearns, Stanhope, & McKinney, 2021). The significance of social support as a protective factor on health both in mentally and physically, in the way that modulating the adverse impact of distressing determinants such as NLEs, have been demonstrated by an ever-growing number of research (Berkman & Glass, 2000; Grey et al., 2020). Its protective benefits provide a coping resource, particularly with stressful events or circumstances (Scheid & Wright, 2017) as well as in the context of infectious disease crises. Research conducted during past pandemics, including not only recent COVID-19 (Szkody et al., 2021) but also Ebola, SARS, HIV/AIDS (Asante, 2012; Chew et al., 2020), and has verified that lower rates of psychiatric disorders were associated with social support.
Studies based on the Stress-buffering hypothesis (Cassel, 1976) demonstrated that social support has assumed as a protective factor which buffers the adverse impact of distressing stressors on one’s health and wellbeing, such as NLEs. When individuals have or perceive more available social support or resources, the stressful event or situation can be better handled with one’s heightened sense of control and enhanced emotional disclosure. This in turn improves associated consequences, such as lowered depression (Szkody & McKinney, 2019) or anxiety and better care service access (Szkody et al., 2021).
It has been theorized that perceived social support (PSS) helps individuals to reappraise the stressful event or situation, while it has been assumed that received support itself fight against the effects of stress by supporting one’s coping mechanism (Cohen, Gottlieb, & Underwood, 2001). The PSS has highlighted by social cognitive theories based on cognitive processes involving support appraisal, which challenges the traditional concept that perceptions of support are basically determined by supportive events which is objective and identifiable (Grey et al., 2020). A meta-analytic research probing the relationship of both kinds of social support indicates only a modest correlation between received support and PSS (Haber, Cohen, Lucas, & Baltes, 2007). In addition, Szkody and McKinney (2019) provided evidence of relatively greater importance of available support perceptions (PSS) rather than received support.
There have been two explanations about how, specifically, social support and psychological health are associated : the first is the main effect model and the second is the buffering model (Scheid & Wright, 2017). The first model presents a theory that perceived social resources are able to directly affect the psychological health. In this perspective, social support is psychologically beneficial by itself, whether or not significant stress is present (Scheid & Wright, 2017). Whereas the second model assumes that the support could play a part in buffering or moderating the impact of life stress (Cassel, 1976). From this point of view, its significance on psychological health tends to be considered to play only a partial role, only to the extent in which social support reduces the distress of stress exposure on psychological well-being (Scheid & Wright, 2017). However, recent researchers have believed the both model of social support are not necessarily mutually exclusive (Berkman & Glass, 2000).
Thus, the current study examined the protective effect of PSS on psychological health among the general population by considering the NLEs during the COVID-19 pandemic in South Korea, which applied a range of long-term containment strategies.
Ⅱ. Methods
1. Research design
This study hypothesizes that depression and embitterment are two key dependent variables as outcomes of stress. One is depression, which occupies a major axis in the psychological health studies of diverse populations as the strongest indicator of suicide risk, and a significant deterioration in the level of depression during the coronavirus pandemic has been reported (WHO, 2022). A strong association between PSS and depression is reported (Henderson, 1992), which is particularly effective in reducing levels of depressive symptoms in situations of greater exposure to stressors (Burton, Stice, & Seeley, 2004). Therefore, depression and its expected strong correlation with PSS is considered as a priority in the current research.
The other dependent variable of the current study (i.e., embitterment) has also been shown to be important in recent psychological research (Linden, 2017). Embitterment is a mixed-up emotion characterized as “a nagging and burning feeling of being let down, insulted, or being a loser, and of being revengeful but helpless (Linden, 2017),” which is triggered after experiencing NLEs. The often accompanied characteristic of those events is the unjust or insulting experience partnered with violating basic beliefs and values (Linden et al., 2008). Increased rates of embitterment of the general population in Europe have been observed during the coronavirus pandemic (Muschalla, Vollborn, & Sondhof, 2021). The emotional state during the coronavirus pandemic was distinguished clearly from other clinically relevant psychological health outcomes (Muschalla et al., 2021). Embitterment can be pathogenic and fall into post-traumatic embitterment disorder (PTED), an adjustment disorder with long-lasting and disabling symptoms and psychological reactions as manifestation (Linden et al., 2008).
The characteristics of embitterment distinguished from major depressive symptoms include feelings of injustice, humiliation, and insults by external stressors (e.g., insurance company employees), which showed changes in affect such as becoming comforted when thinking of revenge (Ko, Han, & Chae, 2014). It also is characterized as externalizing the cause of stress and victimizing oneself (Linden et al., 2008). On the other hand, characteristics of depression include internalizing the cause of stress with symptoms of sadness, difficulty making decisions, lack of energy, and self-criticism accompanying impaired affect modulation (Lopez Molina et al., 2014). Thus, it can be assumed that the link between PSS and depression might be stronger than that of embitterment (Henderson, 1992).
Therefore, the specific hypotheses that we examined in this study are as follows:
1) Greater levels of NLEs during the coronavirus pandemic will be associated with higher levels of psychological health (depression and embitterment, respectively), in consideration of PSS.
2) Higher levels of PSS will be linked with lower levels of psychological health (depression and embitterment, respectively), in consideration of the experience of NLEs.
3) The surmised protective effects of PSS in hypothesis 2 will be stronger in depression than in embitterment.
2. Participants
Research participants were the community residents 18 years of age or older in Gyeonggi province, South Korea. As a local government, Gyeonggi Province is largest with 13 million residents in Korea. It has heterogeneity in mixed urban and rural areas with a high density of housing and industries. Gyeonggi Province can be said to be a miniature version of Korea nationwide that has 31 basic local governments with various forms, financial independence, self-reliance, and large population. To date, the overall mental health of residents in Gyeonggi Province during COVID-19 has been similar to or slightly better than the national level (KCDC, 2022).
This study is approved by the institutional review board of Seoul National University (IRB No. 2201/002-008). An online survey was conducted to the participants who provided informed consent by an investigation firm in Korea (Hankook Research, Inc.). The participants anonymously answered a structured survey questionnaire from January 18th to 26th, 2022. For ensuring the study population’s proportionate ratio in data collection, we adopted a quota sampling method with regard to age, gender, and 8 residential areas of Gyeonggi province based on the status of the national resident population in January 2022. For quality assurance, incomplete data were excluded ay the data modification, and 1,000 sample were utilized in the analysis.
The complete sample dataset included 495 females (49.5%) and most respondents were above 60 years of age or in their 50s (25.3%; 20.1%) followed by respondents in 40s (19.5%), 20s (18.2%), and 30s (16.5%). Most respondents (76.9%) had a college education or higher education and 23.1% of respondents reported a high school education or lower. The largest proportion of the monthly household income for the participants was 3.00-5.00 million won ($2,201-$3,668; 28.0%) followed by 7.00 million won ($5,136) or more (26.8%), 5.00 -7.00 million won ($3,668-$5,136; 24.9%), and less than 3.00 million won (less than $2,201; 20.3%), respectively.
3. Measures
Depression and embitterment were included as dependent variables. Depression of the participants was measured using the Korean version of Patient Health Questionnaire-9 (PHQ-9). The 9 items in the questionnaire assessed the frequency of depressive symptoms over the past two weeks using a 4-point Likert scale (“rarely or none of the time” to “most or all of the time”). The aggregated score consists of 0-27 points, whereby the higher the score, the more intense the symptoms of depression. The level of participants’ depression was classified based on the PHQ-9 cutoff score greater than or equal to 10 points implying the existence of depression (Ko et al., 2014). The inter-item reliability was desirable (Cronbach’s α=0.92). In the hypothesis examination, the sum score of PHQ-9 was put into the analysis as a continuous variable.
Embitterment of the participants was measured with the posttraumatic embitterment disorder (PTED) self-rating scale (Linden, Baumann, Lieberei, & Rotter, 2009; Shin et al., 2012) consisting of a 5-point Likert scale (“not true at all” to “extremely true”). It assesses individual’s prolonged, disabling embitterment reactions in the aftermath of NLEs by means of 19 items. The level of embitterment based on the response results can be classified as in a normal state if the mean score is below 1.6 points, a chronic state if the score is above 1.6 and below 2.5 points, and a clinically significant levels of embitterment in case the mean point is 2.5 or higher (Linden et al., 2009). The inter-item reliability was excellent (Cronbach’s α=.97). The average score was used for the hypothesis examination as a continuous variable.
The independent variable of interest in this research was NLEs during COVID-19. To measure the experiences of NLEs during COVID-19, a total of 11 items from Brugha and Cragg (1990)’s original negative life event list were used, which were adopted in respect to recent social issues and context of South Korea. The time interval of experiencing NLEs was questioned from January 20, 2020 (the date of COVID-19 outbreaks in South Korea) to the time of this investigation. The items included life experiences such as significant economic crisis, job loss (closure) or employment failures, marital separation (divorce), broken intimate relationship with close relations, death of family member or friend, personal or close people’s physical harm (disease, injury, or violence) and others. A nominal scale was used to assess the negative experiences of the respondents (1=“not experienced”; 2=“experienced”). The inter-item reliability was acceptable (Cronbach’s α=.75).
The PSS was measured using 6 items of Medical Outcomes Study Social Support Survey’s (MOS-SSS-6; Holden, Lee, Hockey, Ware, & Dobson, 2014). The items were assessing about how often someone is available in support needed situations using a 5-point Likert scale (“none of the time” to “all of the time”). The support situations included such as “getting along with for relaxation,” “taking me to the doctor if needed,” “sharing my most private worries and fears,” “seeking advice on problems,” “doing something enjoyable with me,” and “loving me and making me feel wanted.” The inter-item reliability was desirable (Cronbach’s α=.94).
The sociodemographic characteristics (gender, age, education level, and monthly household income) of the participants were controlled as covariates. The general and governmental trust variables measured using a 4-point Likert scale, which could affect the result as a potential buffering resource, were also controlled. The experience of COVID-19 confirmation and self-isolation of the participants measured nominally was applied as covariates in consideration of the pandemic situation. A control for justice belief assessed by a personal BJW scale (Dalbert, 1999) was also applied that could function as confounders, particularly in the analysis of embitterment results.
4. Statistical analysis
Data were analyzed using the SAS 9.5 and SPSS 25 software utilizing bootstrap methods (10,000 bootstraps). After calculating the initial descriptive analysis and correlation analysis for the study variables, the hypotheses were examined by a hierarchical regression with embitterment and depression as the dependent variables, respectively. The first step included covariates which had possible confounding effects pertaining to embitterment and depression. The covariates included participants’ sociodemographic status, governmental and general trust, justice belief, COVID-19 confirmation, and self-isolation experience. The second step included the effects of the experience of NLEs during COVID-19 and PSS on depression and embitterment, respectively. For the final step, we compared the surmised protective effects of PSS on the depression and embitterment in the second step. The potential multicollinearity was found to be rejected based on the tolerances and VIF values.
Ⅲ. Results
1. Depression and embitterment
The mean score of depression (PHQ-9) was 6.79 (SD=6.10). Based on the definition of depression as having a mean score over 10 points (Ko et al., 2014), 25.1% of the respondents were found to be at depression level. On the other hand, the average embitterment score of the participants was 1.57 (SD=0.80). When applying the cut-off score of the original scale (Linden et al., 2009), the percentage of participants with a “severe embitterment” state at a clinically significant intensity was 10.9%, 34.6% of participants was in a “chronic embitterment” state, and 54.5% of respondents was in a normal state of embitterment. Although there is a limit to the comparison due to sample differences, the prevalence of depression (PHQ score of 10 or higher) from the current study (25.1%) was considerably higher than that of the general population of Korea before the coronavirus epidemic (6.7%; Shin et al., 2017), while the level of embitterment (M=1.57, SD=0.80) has gone down (M=1.73, SD=0.74; You & Ju, 2020).
Subgroup differences in terms of participants’ sociodemographic characteristics were identified conducting an analysis of variance (ANOVA) or t-test for capturing relatively vulnerable groups. The results found significant differences regarding depression based on age; however, results with regard to embitterment were not statistically significant. Depression of younger participants in their 20s (7.30) and 30s (8.28) was significantly higher than in other age groups.
2. NLE experiences during COVID-19 and PSS
The mean score of NLE experiences during COVID-19 was 1.11 (SD=1.66). The most experienced NLE during COVID-19 was “significant economic crisis” (26.2%), followed by “job loss (closure) or employment failures” (26.2%), “broken intimate relationship with close relations” (15.4%), “death of family member or friend” (11.3%), and “close people’s physical harm (disease, injury, or violence)” (8.7%). Differences in the mean scores based on sociodemographic characteristics were not statistically significant.
The average score of PSS was 23.17 (SD=5.41). Among the six support situations provided, the most vulnerable situations based on the 1=“none of the time” response of the 5-point Likert scale were “getting along with for relaxation” (13.3%) and “taking me to the doctor if needed” (10.8%), followed by “sharing my most private worries and fears”(10.3%), “seeking advice on problems” (10.15%), “loving me and making me feel wanted” (8.7%), and “doing something enjoyable with me” (8.1%). The results of the mean scores by sociodemographic characteristics pointed out that the differences in average PSS based on gender and monthly household income were statistically significant; the groups with significantly low PSS levels were male (mean score: 22.77) and low monthly household income group with less than 3 million won (mean score: 21.26).
3. Research hypotheses examination
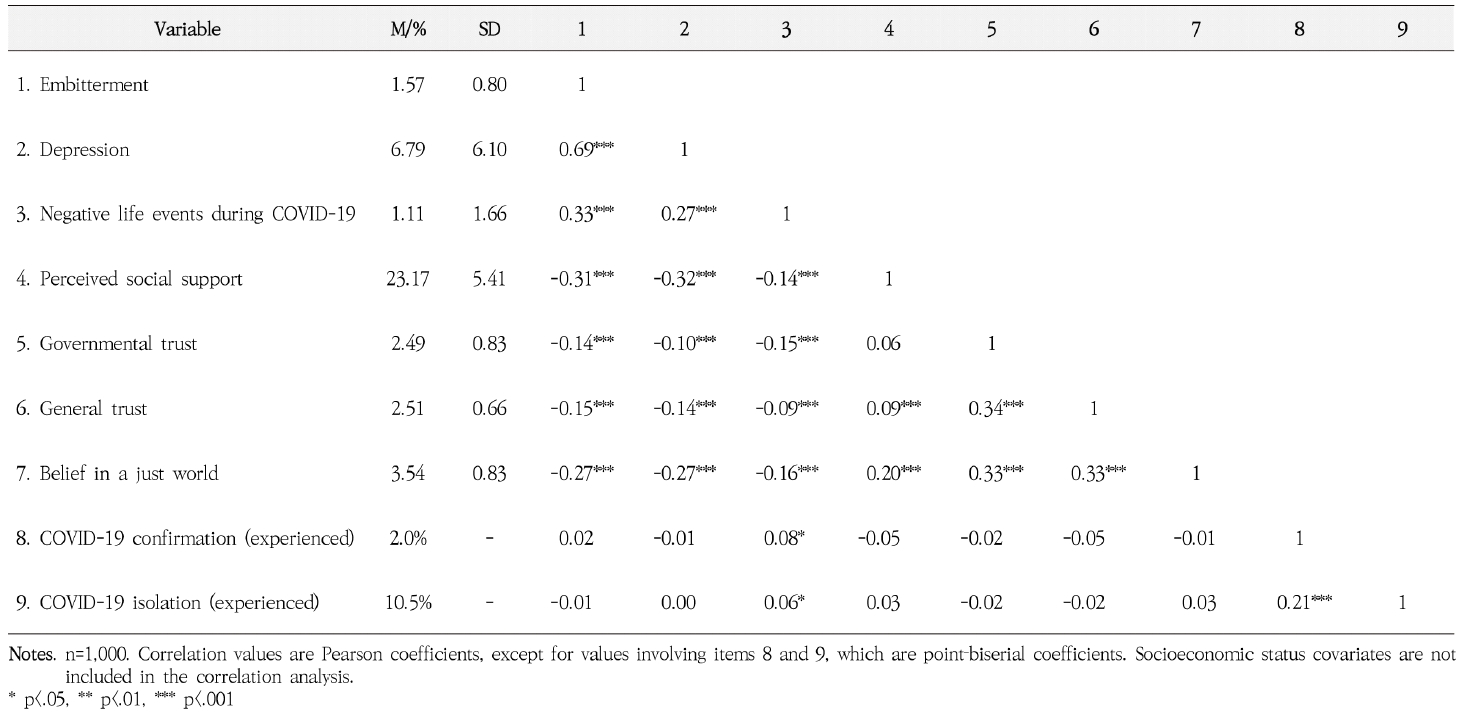
Initial correlation analysis indicated that high NLEs during COVID-19 was associated with increased depression (r=.27, p<.001) and embitterment (r=.33, p<.001). Whereas high PSS was linked with decreased depression (r=-.32, p<.001) and embitterment (r=-.31, p<.001; see Table 1).
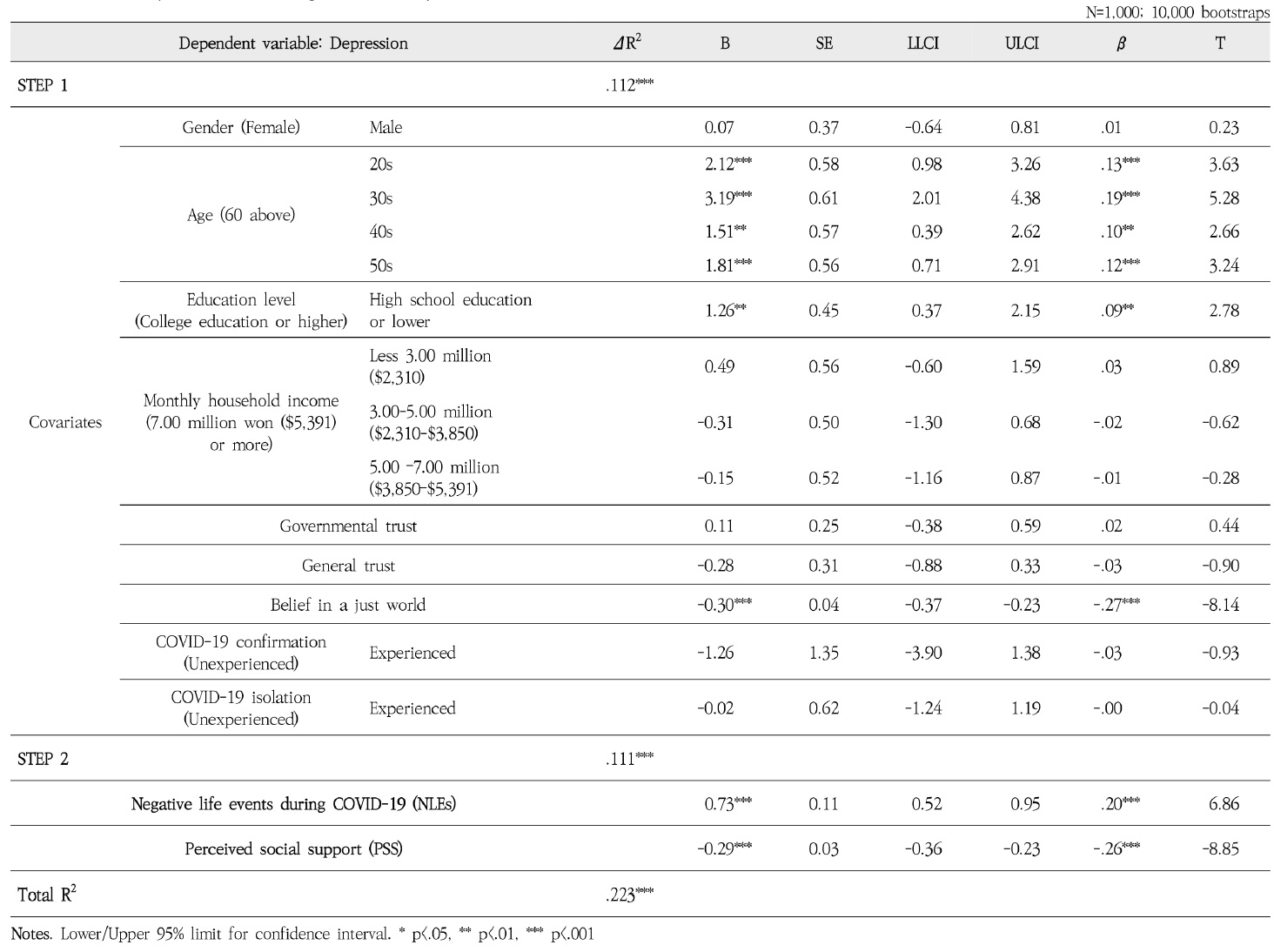
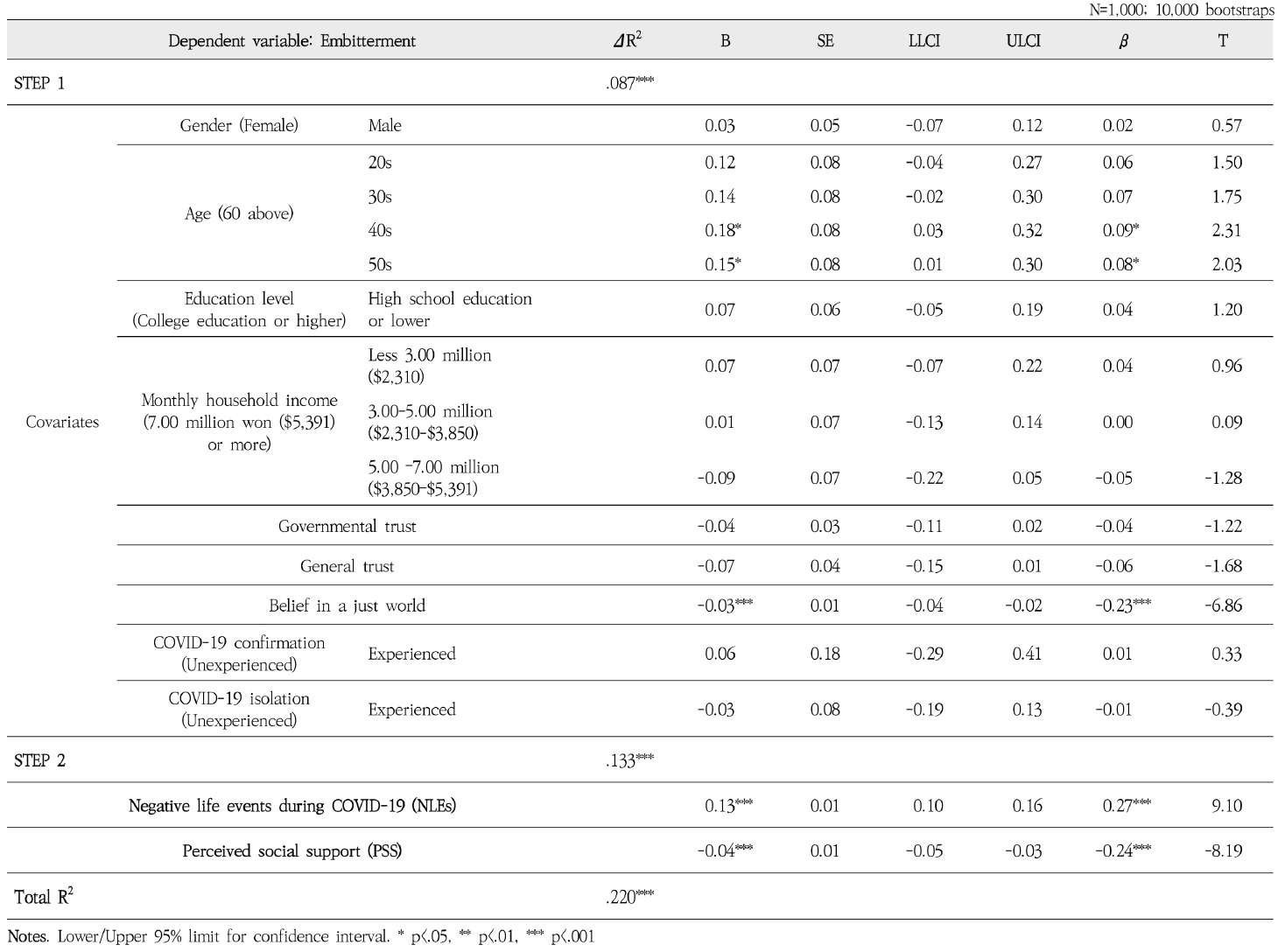
Research hypotheses were examined by a hierarchical regression with embitterment and depression as the dependent variables, respectively. Concerning depression, the regression analysis confirmed a significant effect of NLEs during COVID-19 on depression (B=0.73, SE=0.11, β=.20, p<.001), which is in accordance with the first hypothesis <Table 2>. In respect to the second hypothesis, a significant effect for PSS was verified in connection with depression (B=-0.29, SE=0.03, β=-.26, p<.001) <Table 2>. Thus, the protective effect of PSS on depression, in consideration of the experience of NLEs, was found to be statistically significant. With respect to embitterment, the regression analysis verified a significant effect for both NLEs during COVID-19 (B=0.13, SE=0.01, β=.27, p<.001) and PSS with regard to embitterment (B=-0.04, SE=0.01, β=-.24, p<.001), which is in accordance with the first two hypotheses. These results indicate the significant protective effect of PSS on embitterment <Table 3>.
With respect to the third hypothesis, as expected, the surmised association related to PSS was discovered to be stronger with depression (B=-0.29, SE=0.03, β=-.26, p<.001) than with embitterment (B=-0.04, SE=0.01, β=-.24, p<.001). These results provide evidence that the protective effect of PSS is greater in case of depression rather than in case of embitterment when NLEs during COVID-19 are considered.
Ⅳ. Discussion
This research aims to examine the protective role of PSS and to derive practical implications focusing on its effects on depression and embitterment, in consideration of the NLEs that occurred during the coronavirus pandemic in South Korea.
First, this study confirmed significant protective effects of PSS on depression and embitterment, respectively, in consideration of the experience of NLEs during the COVID-19 pandemic. The results demonstrate higher levels of PSS are connected to lower levels of depression and embitterment. The statistical results are in accordance with studies before the pandemic of protective effect of PSS showing that social support is effective in reducing depressive symptom levels in situations with greater exposure to stressors (Burton et al., 2004; Szkody & McKinney, 2019) and embitterment (You & Ju, 2020).
The study findings are in agreement with recent research during COVID-19 showing that PSS can improve psychological health (Qi et al., 2020; Song & Yoo, 2020; Szkody et al., 2021). Qi et al. (2020) found adolescents in China who had relatively low levels of social support showed an increased prevalence of psychological disorder during the pandemic. In addition, the link between coronavirus concerns and mental health is buffered by PSS when taking the period of self-isolation into account (Szkody et al., 2021). And, a possibility of a significant protective effect of PSS during the context of coronavirus pandemic in Korea is proposed (Song & Yoo, 2020).
PSS is worthy of attention in the context of the essential relationship resources for well-being during a prolonged COVID-19 pandemic. A range of non-pharmaceutical interventions to “flatten the curve”, including physical distancing and self-isolation, have been implemented. These efforts might be fruitful for diminishing the spread of the virus, but also led to social distancing, not just physical distancing. Reduced social gatherings and connections due to physical distancing and self-isolation following the pandemic could act as risky determinants for the onset and deterioration of psychological health (Grey et al., 2020), which may have raised the estimations of poor psychological health, loneliness, and feelings of isolation during the pandemic (Szkody et al., 2021).
Second, the protective effect of PSS on depression was greater than in the case of embitterment in this study. The results identified differences between depression and embitterment as psycho-social health indicators. Depression accompanies characteristics of internalizing the cause of stress with symptoms of sadness, difficulty making decisions, lack of energy, and self-criticism with impaired affect modulation (Lopez Molina et al., 2014). On the other hand, embitterment characterized as externalizing the cause of stress and victimizing oneself (Linden et al., 2008), thus the protective effect of PSS might not be great as depression. In contrast with depression, unimpaired affect modulation was identified in embittered (PTED) patients whom displaying of a normal/positive affect when they are not attentive or of an emotionally engagement in vengeance fantasies (Linden et al., 2008). In addition, the onset of PTED was directly connected to a single distressing life event (Linden, Baumann, Rotter, & Schippan, 2007). In contrast, for depression, typical NLEs are rather long-lasting strains or are even shown inverse correlative relationships in which earlier depression predicts stressful life events afterwards (Sheehan et al., 1998).
These results are complying with previous studies that PSS protects against the growth of psychiatric disorder in the presence of preceding exposure to stressors to individuals (e.g., NLEs), especially with depression (Burton et al., 2004; Henderson, 1992). In a meta-analysis evaluating 35 research about the connection between depression and social support, most studies observed social support’s significant protective effects (Henderson, 1992). Social support has been effective in reducing depressive symptom levels in situations with greater exposure to stressors (Burton et al., 2004). A low risk of depression was reported in those forming reliable human relationships for diminishing the depression vulnerability due to life events or prolonged life difficulties (Szkody & McKinney, 2019). Another early study demonstrated social support’s protective role against the growth of psychiatric disorder only in the presence of preceding exposure to stressors to individuals (e.g., NLEs), and the protective effect was strong for depression especially (Henderson, 1992).
Third, the results identified an association between higher levels of NLEs during coronavirus pandemic and deteriorated levels of depression and embitterment, respectively. Similar to previous studies, our results confirmed that stressful life events have a role in modulating individual vulnerability to mental health (Linden et al., 2008). Considering the influence of covariates, including sociodemographic characteristics, the results indicate that an individual’s social experience impacted the level of depression and embitterment during the pandemic. When looking at the items of the NLE scale in more detail, the most commonly experienced NLE during COVID-19 was “significant economic crisis” (26.2%), followed by “job loss (closure) or employment failures” (26.2%). These results indicate that social efforts to create jobs, support employment, and financial support for small business owners and low-income households in communities are needed in order to alleviate psychological problems.
In addition, the subgroup analysis showed significantly lower PSS among male and low-income respondents. These results suggest that in order to protect psychological health of the community during the prolonged pandemic, a targeted and integrated approach (social, economic, emotional, and health) should be developed for more vulnerable populations (male and low-income) in order to reduce the negative events and promote social support. Also, efforts are needed to strengthen the screening program to detect at-risk groups and the accessibility of mental health services to help people better cope with life stresses.
There are several limitations to this study. First, there remain open questions about the difference between depression and embitterment related to stress-buffering mechanisms. Thus, further studies, such as a multi-group analysis that considers significant covariates of age (depression, embitterment) and educational level (depression), as well as further verification, such as whether the results are due to the specific situation of the coronavirus pandemic, are required to better understand the study findings. Second, the research design was cross-sectional utilizing a local provincial level data based on a quota sampling, so further research effort is necessary for better understanding about the longitudinal relationships among the study variables. Third, it is possible that the study data were the result of a common method bias.
Practical implications for public health promotion uncovered from the study findings are as undermentioned. First, given the significant effect of PSS on depression and embitterment from cases in Korea during the coronavirus pandemic, which required a range of long-term containment strategies limiting individual daily life, effort from the international community is needed to develop strategies that can reduce the detrimental impact on psychological health and promote social support. These include strategies using safe offline meetings or supportive online meetings/contacts based on scientific and technological development that can protect connectivity resources at the interpersonal level, and mental health advocacy strategies at the community and policy level, for not only COVID-19, but also other possible infectious disease pandemic. Second, non-pharmaceutical interventions, such as physical distancing, are inevitable in testing, tracing, and quarantine (TTQ) during pandemics, but physical distancing should be distinguished from "social" distancing and would not be converted to it. A decrease in the level of PSS should also be prevented due to unnecessary (excessive) social distancing such as indiscriminate shutdown time policies without thorough consideration of the characteristics of policy subject. Moreover, a targeted and integrated approach (social, economic, emotional, and health) should be developed for more vulnerable populations (male and low-income) in order to reduce negative events and promote social support. Our study underscores the need to strengthen screening of various psychological health issues in communities based on the results of different protective effects of PSS for depression and embitterment.
Ⅴ. Conclusion
This study analyzed cases in South Korea, in which long-term containment strategies were applied during the coronavirus pandemic, to examine the protective role of PSS regarding depression and embitterment, in consideration of the NLEs during the COVID-19 pandemic. The results showed that the higher levels of the NLEs during the pandemic are associated with deteriorated levels of depression and embitterment, respectively. The protective effects of the PSS on depression and embitterment were confirmed in consideration of the NLEs during the COVID-19 pandemic, which had a greater impact on depression than in the case of embitterment. This study underlines the need for social efforts to develop targeted and integrated strategies that take PSS into account in the ongoing and future pandemic to minimize detrimental effects on psychological health.
Acknowledgments
This work was supported by the Gyeonggi Infectious Disease Control Center of the Gyeonggi Provincial Government, and the National Research Foundation of Korea (BK21 Center for Integrative Response to Health Disasters, Graduate School of Public Health, Seoul National University)(NO.419 999 0514025).
References
-
Asante, K. O. (2012). Social support and the psychological wellbeing of people living with HIV/AIDS in Ghana. African Journal of Psychiatry, 15(5), 340-345.
[https://doi.org/10.4314/ajpsy.v15i5.42]

- Berkman, L. F., & Glass, T. (2000). Social integration, social networks, social support, and health. In L. F. Berkman, & I. Kawachi (Eds.), Social Epidemiology (pp. 137-173). United Kingdom, UK: Oxford University Press.
-
Brugha, T. S., & Cragg, D. (1990). The list of threatening experiences: The reliability and validity of a brief life events questionnaire. Acta Psychiatrica Scandinavica, 82, 77-81.
[https://doi.org/10.1111/j.1600-0447.1990.tb01360.x]

-
Burton, E., Stice, E., & Seeley, J. R. (2004). A prospective test of the stress-buffering model of depression in adolescent girls: No support once again. Journal of consulting and clinical psychology, 72(4), 689.
[https://doi.org/10.1037/0022-006X.72.4.689]

-
Cassel, J. (1976). The contribution of the social environment to host resistance: The fourth wade hampton frost lecture. American Journal of Epidemiology, 104(2), 107-123.
[https://doi.org/10.1093/oxfordjournals.aje.a112281]

-
Chew, N. W., Lee, G. K., Tan, B. Y., Jing, M., Goh, Y., Ngiam, N. J., . . . Shanmugam, G. N. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity, 88, 559-565.
[https://doi.org/10.1016/j.bbi.2020.04.049]

- Cohen, S., Gottlieb, B. H., & Underwood, L. G. (2001). Social relationships and health: Challenges for measurement and intervention. Advances in Mind-Body Medicine, 17(2), 129-141.
-
Dalbert, C. (1999). The world is more just for me than generally: About the personal belief in a just world scale's validity. Social Justice Research, 12(2), 79-98.
[https://doi.org/10.1023/A:1022091609047]

-
Grey, I., Arora, T., Thomas, J., Saneh, A., Tohme, P., & Abi-Habib, R. (2020). The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Research, 293, 113452.
[https://doi.org/10.1016/j.psychres.2020.113452]

-
Haber, M. G., Cohen, J. L., Lucas, T., & Baltes, B. B. (2007). The relationship between self-reported received and perceived social support: A meta-analytic review. American Journal of Community Psychology, 39(1-2), 133-144.
[https://doi.org/10.1007/s10464-007-9100-9]

- Henderson, A. (1992). Social support and depression. In H. O. F. Veiel, & U. Baumann (Eds.), The meaning and measurement of social support (pp. 85-92). New York, NY: Hemisphere Publ Corp.
-
Holden, L., Lee, C., Hockey, R., Ware, R. S., & Dobson, A. J. (2014). Validation of the MOS Social Support Survey 6-item (MOS-SSS-6) measure with two large population-based samples of Australian women. Quality of Life Research, 23(10), 2849-2853.
[https://doi.org/10.1007/s11136-014-0741-5]

- Korea Disease Control and Prevention Agency [KCDC]. (2022). 2021 Community Health Survey. Sejong: Ministry of Health and Welfare of Korea. Retrieved from https://chs.kdca.go.kr/chs/main.do
- Ko, H., Han, C., & Chae, J. (2014). Understanding of posttraumatic embitterment disorder (PTED). Anxiety and Mood, 10(1), 3-10.
-
Linden, M. (2017). Definition and assessment of disability in mental disorders under the perspective of the international classification of fnctioning disability and health (ICF). Behavioral Sciences & the Law, 35(2), 124-134.
[https://doi.org/10.1002/bsl.2283]

-
Linden, M., Baumann, K., Lieberei, B., & Rotter, M. (2009). The post-traumatic embitterment disorder self-rating scale (PTED Scale). Clin Psychol Psychother, 16(2), 139-147.
[https://doi.org/10.1002/cpp.610]

-
Linden, M., Baumann, K., Rotter, M., & Schippan, B. (2007). The psychopathology of posttraumatic embitterment disorders. Psychopathology, 40(3), 159-165.
[https://doi.org/10.1159/000100005]

-
Linden, M., Baumann, K., Rotter, M., & Schippan, B. (2008). Posttraumatic embitterment disorder in comparison to other mental disorders. Psychotherapy and Psychosomatics, 77(1), 50-56.
[https://doi.org/10.1159/000110060]

-
Lopez Molina, M. A., Jansen, K., Drews, C., Pinheiro, R., Silva, R., & Souza, L. (2014). Major depressive disorder symptoms in male and female young adults. Psychology, Health & Medicine, 19(2), 136-145.
[https://doi.org/10.1080/13548506.2013.793369]

-
Muschalla, B., Vollborn, C., & Sondhof, A. (2021). Embitterment as a specific mental health reaction during the coronavirus pandemic. Psychopathology, 54(5), 232-241.
[https://doi.org/10.1159/000517447]

-
Qi, M., Zhou, S.-J., Guo, Z.-C., Zhang, L.-G., Min, H.-J., Li, X.-M., & Chen, J.-X. (2020). The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. Journal of Adolescent Health, 67(4), 514-518.
[https://doi.org/10.1016/j.jadohealth.2020.07.001]

-
Rossi, R., Jannini, T. B., Socci, V., Pacitti, F., & Lorenzo, G. D. (2021). Stressful life events and resilience during the COVID-19 lockdown measures in Italy: Association with mental health outcomes and age. Front Psychiatry, 12, 635832.
[https://doi.org/10.3389/fpsyt.2021.635832]

-
Santomauro, D. F., Herrera, A. M. M., Shadid, J., Zheng, P., Ashbaugh, C., Pigott, D. M., . . . Aravkin, A. Y. (2021). Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet, 398(10312), 1700-1712.
[https://doi.org/10.1016/S0140-6736(21)02143-7]

-
Scheid, T. L., & Wright, E. R. (2017). A handbook for the study of mental health. United Kingdom, UK: Cambridge University Press.
[https://doi.org/10.1017/9781316471289]

- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., . . . Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry, 59 (Suppl 20), 22-33.
-
Shin, C., Han, C., Linden, M., Chae, J., Ko, Y., Kim, Y., . . . Jung, I. (2012). Standardization of the Korean version of the posttraumatic embitterment disorder self-rating scale. Psychiatry Investigation, 9(4), 368.
[https://doi.org/10.4306/pi.2012.9.4.368]

-
Shin, C., Kim, Y., Park, S., Yoon, S., Ko, Y., Kim, Y., . . . Han, C. (2017). Prevalence and associated factors of depression in general population of Korea: Results from the Korea national health and nutrition examination survey, 2014. Journal of Korean Medical Science, 32(11), 1861-1869.
[https://doi.org/10.3346/jkms.2017.32.11.1861]

-
Song, E., & Yoo, H. J. (2020). Impact of social support and social trust on public viral risk response: A COVID-19 survey study. International Journal of Environmental Research and Public Health, 17(18), 6589.
[https://doi.org/10.3390/ijerph17186589]

-
Szkody, E., & McKinney, C. (2019). Stress-buffering effects of social support on depressive problems: Perceived vs. received support and moderation by parental depression. Journal of Child and Family Studies, 28(8), 2209-2219.
[https://doi.org/10.1007/s10826-019-01437-1]

-
Szkody, E., Stearns, M., Stanhope, L., & McKinney, C. (2021). Stress‐buffering role of social support during COVID‐19. Family Process, 60(3), 1002-1015.
[https://doi.org/10.1111/famp.12618]

- World Health Organization [WHO]. (2022). Mental health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief, 2 March 2022 (No. WHO/2019-nCoV/Sci_Brief/Mental_health/2022.1). World Health Organization.
-
You, M., & Ju, Y. (2020). Modeling embitterment dynamics: The influence of negative life events and social support mediated by belief in a just world. Journal of Affective Disorders, 274, 269-275.
[https://doi.org/10.1016/j.jad.2020.05.108]